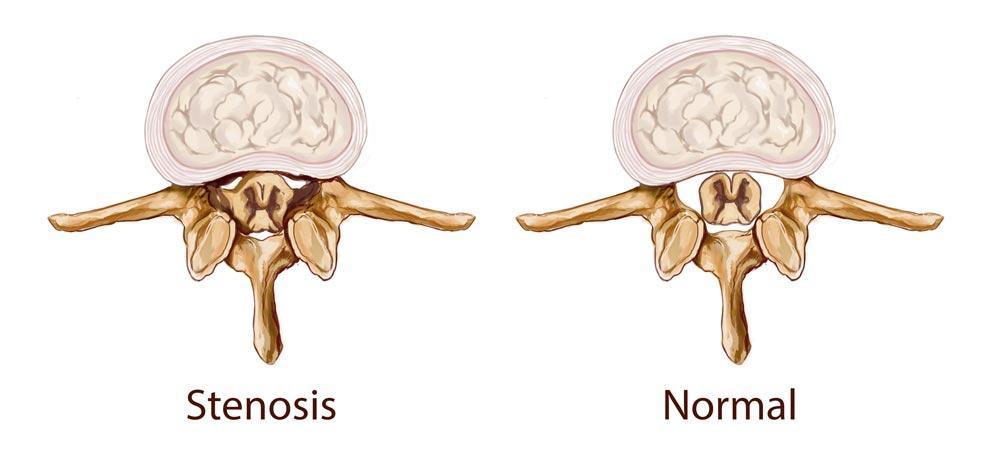
Spinal stenosis is a condition in which one or more of the spine’s bony openings, called foramina, narrow. There are two types.
Central canal stenosis occurs when the spinal canal narrowing places pressure on the spinal cord.
Lateral stenosis is when the nerve roots in the intervertebral bony openings where nerves branch off the spinal cord are inflamed or compressed. The pinched or compressed nerves or spinal cord can cause back pain burning pain that shoots down the legs, numbness, tingling or weakness in the legs or feet, or more severe symptoms. Following are seven common questions people have about spinal stenosis.
1. How Common is Spinal Stenosis?
Though spinal stenosis can develop anything along the spine, lumbar spinal stenosis is the most common. The reason is that the nerve root area naturally decreases in the lower (lumbar) spine. It is most common in people over 50 years old because it is a degenerative change. The American Academy of Orthopedic Surgeons says that up to 95 percent of people over 50 years old will experience degenerative spine changes. Spinal stenosis develops most frequently in men and women over 60 years old.
2. What is the Most Common Cause of Spinal Stenosis?
Though anyone can develop spinal stenosis, it usually develops as people age. The most common cause of spinal stenosis, according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, is aging which leads to changes in the spine over time. The other common causes of spinal stenosis are osteoarthritis and rheumatoid arthritis. In some cases, collapsing spinal disc space is due to a condition like a bulging disc.
3. What is Severe Spinal Stenosis?
Severe spinal stenosis is when the narrowing of the spinal canal causes symptoms like pain or numbness in the legs and feet that make walking extremely difficult or almost impossible. Spinal stenosis can also lead to cauda equina syndrome, in which multiple nerve roots are damaged or irritated, causing severe symptoms.
Cauda equina is the collection of nerves at the end of the spinal cord responsible for the nerves sending and receiving signals back and forth from the lower limbs and pelvic organs. Severe spinal stenosis can lead to bladder or bowel problems, loss of sensation in the buttocks, genital area and inner thighs, sexual dysfunction, sciatica, and/or paralysis of a nerve root. Eventually, cauda equina syndrome may cause permanent nerve damage.
4. How is Spinal Stenosis Treated?
Spinal stenosis is first treated with non-surgical options that include anti-inflammatory and pain medications, physical thearpy, epidural injections, or a combination of various treatments. You may find some relief by leaning forward while walking, sitting or doing other activities because flexing forward can open up some of the spine’s spaces between the joints. Various surgical procedures are possible if the condition does not adequately respond to non-surgical treatments. Your doctor will develop a spinal stenosis treatment plan based on the results of the diagnostic procedures performed.
Louisiana Pain Specialists is proud to offer the most advanced therapies, treatments, and technologies to help treat our patients’ pain. We are among the limited pain centers in the Gulf Coast region to offer the Vertiflex procedure for treatment of lumbar spinal stenosis. Designed with patient safety and comfort in mind, this FDA-approved, outpatient procedure offers patients suffering from lumbar spinal stenosis a minimally-invasive alternative to other, more intense surgical options, such as a laminectomy or spinal fusion.
As a safer alternative to traditional, more-invasive surgeries, the Vertiflex procedure involves placing a small implant, or spacer the size of a dime, between the spinous processes of the spine, which are the thin, bony projections on the back of the spine. After the spacer is placed, there is more space for your spinal cord and nerves. The spacer holds the compressed vertebrae further apart which lifts pressure off the nerves to alleviate low back and leg pain.
5. Can Spinal Stenosis Be Cured?
Spinal stenosis cannot be cured, but it can be managed. Always follow the treatment plan your doctor recommends to find relief from pain and improve movement. Following the treatment plan can also slow the condition’s progression or even prevent spinal stenosis from worsening. Regular exercise is essential because it can strengthen your back muscles and ligaments and give your spine more support. It is also important to maintain a healthy weight.
6. What Are the Final Stages of Spinal Stenosis?
Spinal stenosis usually develops slowly. If left untreated, the space in the spinal canal or the intervertebral bony openings will continue to narrow. In the final stages, you will lose control of the bladder and/or bowel, be unable to walk or stand and experience extreme pain or numbness in the lower parts of the body.
Your doctor will grade the severity of your spinal stenosis. Grade is severe lumbar stenosis on a scale of zero to three. At this grade, there is little or no separation in the space where the spinal stenosis is located. If you need surgery because the non-surgical treatments do not work, you are in the final stages of spinal stenosis.
7. How Long Can You Live With Spinal Stenosis?
Spinal stenosis does not shorten life, but it can lead to disability without treatment. A follow-up study of elderly patients who underwent lumbar spine surgery found that patients 60-70 years old had an 87.8 percent survival rate of 10 years.
Early Diagnosis is Important
The most important step you can take when experiencing back or leg problems is to see a doctor for evaluation. The earlier spinal stenosis is diagnosed, the more likely you can live a normal life without fear of disability. There is no cure for spinal stenosis, but you can manage it by rigorously following a treatment plan. If you are experiencing symptoms like back pain, leg numbness or shooting pain down one or both legs, consult our physicians, Dr. Suneil “Neil” Jolly, Dr. Erik Davis, Dr. Eric Sterne, Dr. John Crosby, or Dr. Joshus Kaufman for a diagnosis and treatment plan.