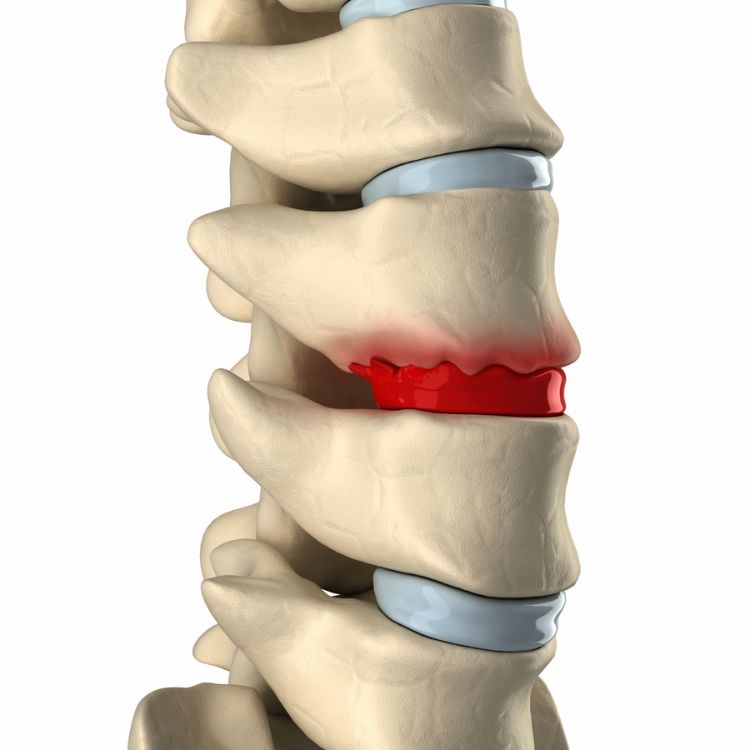
Causes and Symptoms of Degenerative Disc Disease
Symptoms
Not everyone with degenerative disc disease experiences noticeable symptoms. However, for those who do, the most common signs include:
- Lower back pain that may radiate to the buttocks and upper thighs (sciatica)
- Neck pain that may spread to the shoulders and arms
- Stiffness and reduced flexibility in the spine, making bending or twisting painful
- Pain that worsens with prolonged sitting, standing, or movement
- Episodes of intense pain that come and go over time
Some individuals also experience numbness, tingling, or weakness in the arms or legs, particularly if a damaged disc is compressing a nearby nerve.
Causes of Degenerative Disc Disease
Degenerative Disc Disease primarily results from the natural aging process, but other factors can accelerate its progression, including:
- Disc dehydration and thinning – As we age, the spinal discs lose water content, reducing their ability to absorb shock and cushion the vertebrae.
- Repetitive stress and strain – Years of everyday movements, such as bending, twisting, and lifting, contribute to gradual wear on the discs.
- Trauma or injury – High-impact activities, sports injuries, or car accidents can cause sudden or premature disc degeneration.
- Genetics – Some individuals may be genetically predisposed to faster disc degeneration.
- Poor posture and lifestyle habits – Obesity, smoking, and lack of exercise can weaken the spine and accelerate disc breakdown.
How Is Degenerative Disc Disease Diagnosed?
To diagnose degenerative disc disease, a doctor will begin with:
- A thorough medical history and physical exam to assess symptoms, nerve function, and spinal mobility.
- Imaging tests, such as X-rays, MRIs, or CT scans, to evaluate disc health and check for disc thinning, bulging, or herniation.
- Discography, a specialized diagnostic procedure where dye is injected into the discs to identify damage and pinpoint the source of pain.
Treatment Options for Degenerative Disc Disease
There is no cure for degenerative disc disease, but several non-surgical and interventional treatments can help manage symptoms and improve mobility.
Non-Surgical Treatments
- Medications – Over-the-counter pain relievers (NSAIDs) or prescription medications may help reduce inflammation and discomfort.
- Physical Therapy – A structured exercise program strengthens the core, stabilizes the spine, and improves flexibility.
- Heat and Ice Therapy – Applying heat can relax tight muscles, while ice can reduce inflammation and numb pain.
- Lifestyle Modifications – Maintaining good posture, staying active, and avoiding prolonged sitting or heavy lifting can prevent worsening symptoms.
Interventional Pain Management
For individuals with persistent or severe pain, additional treatments may be necessary:
- Epidural Injections – Steroid injections can reduce inflammation and provide temporary relief from pain.
- Nerve Blocks – These injections target specific nerves to interrupt pain signals.
- Minimally Invasive Procedures – In severe cases, procedures such as spinal decompression or disc replacement surgery may be considered.